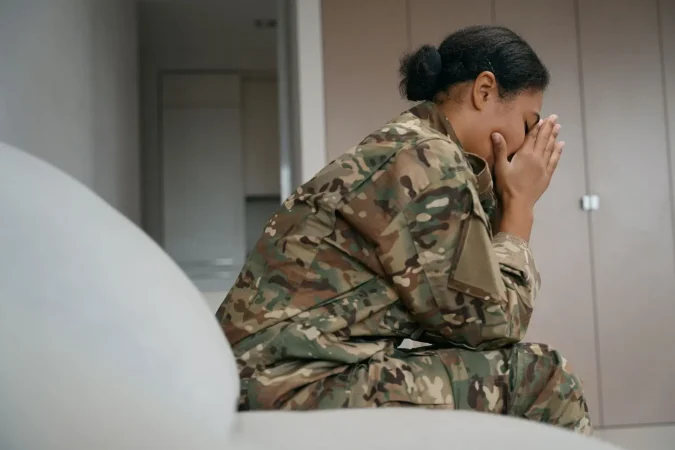
Supporting a veteran with bipolar disorder can feel overwhelming, but it is also one of the most meaningful things you can do for a loved one. At Safe & Sound Treatment, we understand how complex and deeply personal this journey is. Our focus is on offering educational resources, guidance, and comprehensive care to help families navigate the challenges of mental health—especially those linked to military service. This article will provide strategies and insights for helping veterans manage bipolar disorder effectively, emphasizing compassion, patience, and evidence-based care.
Understanding Bipolar Disorder in Veterans
Bipolar disorder is a serious mental health condition that causes extreme mood swings, including manic episodes, hypomania, and depressive episodes. While the general population may struggle with this disorder, veterans face unique risk factors due to their military service. Exposure to trauma, combat, and long periods of stress can exacerbate symptoms or make diagnosis more difficult.
There are different types of bipolar disorder:
- Bipolar I: Involves severe manic episodes often lasting at least a week, followed by depressive episodes.
- Bipolar II: Characterized by less severe hypomanic episodes alongside intense depressive symptoms.
- Cyclothymic Disorder: A milder but chronic form involving frequent mood fluctuations.
Veterans with bipolar disorder may experience rapid shifts in mood, racing thoughts, difficulty sleeping, impulsive behaviors, and periods of deep depression. These symptoms can severely impact daily living, job stability, and social relationships.
Why Veterans Are Especially Vulnerable
Veterans may develop bipolar disorder for a variety of reasons, including:
- Traumatic experiences during combat or training
- High-stress environments and prolonged deployments
- Co-occurring conditions such as post-traumatic stress disorder (PTSD)
- Physical injuries or traumatic brain injury (TBI)
- Genetic predisposition
The stigma around mental illness in military culture can delay diagnosis and treatment, making it even harder for veterans to seek help early on. As a result, many veterans do not receive the care they need until symptoms become severe.
Recognizing the Symptoms
It’s essential to recognize the symptoms of bipolar disorder early so that proper treatment can begin. These symptoms can vary from person to person and across episodes:
Manic Episodes:
- Elevated or irritable mood
- Increased energy levels
- Decreased need for sleep
- Racing thoughts or pressured speech
- Impulsivity or reckless behavior
Depressive Episodes:
- Persistent sadness or feelings of worthlessness
- Fatigue and low energy
- Trouble sleeping or sleeping too much
- Thoughts of death or suicidal ideation
- Difficulty concentrating
Many veterans also experience panic attacks, anxiety, and co-occurring substance use disorders.
How Family Members Can Help
If you’re a family member, friend, or caregiver of a veteran with bipolar disorder, your support can make a crucial difference. Here are some ways you can help:
- Educate Yourself: Learn about the symptoms of bipolar disorder and how it manifests differently in veterans.
- Encourage Treatment: Help your loved one explore treatment options such as therapy, medication, or support groups.
- Be Patient: Mood swings can be hard to manage. Avoid taking things personally during manic or depressive episodes.
- Create Structure: Establishing daily routines can provide stability.
- Practice Active Listening: Sometimes, just being there without judgment can be incredibly healing.
- Promote Self-Care: Encourage healthy habits like regular sleep, physical activity, and mindfulness practices.
Treatment Options for Bipolar Disorder
There are several evidence-based treatments available for bipolar disorder. Many of these options are covered by the U.S. Department of Veterans Affairs (VA):
- Medication: Mood stabilizers, antipsychotics, and antidepressants are often prescribed.
- Psychotherapy: Cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and family-focused therapy are common approaches.
- Hospitalization: Inpatient care may be needed during acute manic or depressive episodes.
- Outpatient Programs: Partial hospitalization and intensive outpatient programs offer structured support.
- Support Groups: These can provide a sense of community and reduce feelings of isolation.
The VA offers a wide range of mental health services and may also provide service-connected disability ratings, which can impact VA benefits and access to care.
Navigating VA Resources
Accessing VA healthcare can be a challenge, but understanding the system is key. Here are some important considerations:
- VA Disability Benefits: Veterans diagnosed with bipolar disorder may qualify for a VA disability rating. The severity of impairment influences the percentage of benefits.
- VA Health Care Enrollment: Eligible veterans can apply for VA health care to access mental health services, medications, and therapy.
- Service-Connected Claims: If the bipolar disorder is related to military service, a claim can be filed for a service-connected disability.
- Medical Records: Keeping detailed records can help during the VA claim process.
Resources such as the VA website (va.gov), county VA offices, or nonprofit outreach programs can assist with navigation and application support.
Addressing the Stigma
Stigma remains a significant barrier to treatment for many veterans. It’s essential to normalize mental health challenges and promote open conversations. Public awareness campaigns, peer support, and transparent communication can all play a role in reducing stigma.
Encouraging a loved one to seek help is not a sign of weakness—it’s an act of strength. Offering understanding instead of judgment can lead to a stronger support system and better outcomes.
When to Seek Emergency Help
If a veteran is experiencing suicidal thoughts, hallucinations, or aggressive behavior, immediate intervention may be necessary. Call 911 or the Veterans Crisis Line at 1-800-273-8255 and press 1.
Other signs that require urgent care:
- Sudden mood changes or erratic behavior
- Refusal to eat, drink, or sleep
- Self-harm or suicidal ideation
- Confusion or disorientation
Emergency rooms and VA medical centers are equipped to handle mental health crises and can initiate stabilization.
Final Thoughts: Support and Healing Are Possible
Living with bipolar disorder can be deeply challenging for veterans, but healing is possible with the right care and support. As a loved one, your role is pivotal. Understanding the condition, encouraging professional help, and remaining a steady presence can change the trajectory of someone’s recovery.
At Safe & Sound Treatment, we specialize in supporting veterans and their families through compassionate, customized care. Whether your loved one is just beginning to explore treatment or needs a higher level of care, our team of professionals is here to help you navigate each step.
Together, we can honor their service by helping them achieve lasting mental wellness.